Using Objective Gait Data to Improve Fall Risk Identification and Prevention
The Unique Role of Data in Fall Prevention
Falls are a significant safety concern, especially for older adults and individuals who have experienced a stroke. Proactively identifying and addressing fall risk is vital when working with patients, as falls are associated with injury, reduced independence, increased caregiver burden, and mortality.
Although fall prevention initially seems simple, many factors contribute to falls, making it difficult to fully predict who is at risk and what strategies will successfully reduce that risk for individuals. Each year, about $50 billion is spent on medical costs related to non-fatal fall injuries, and $754 million is spent related to fatal falls.
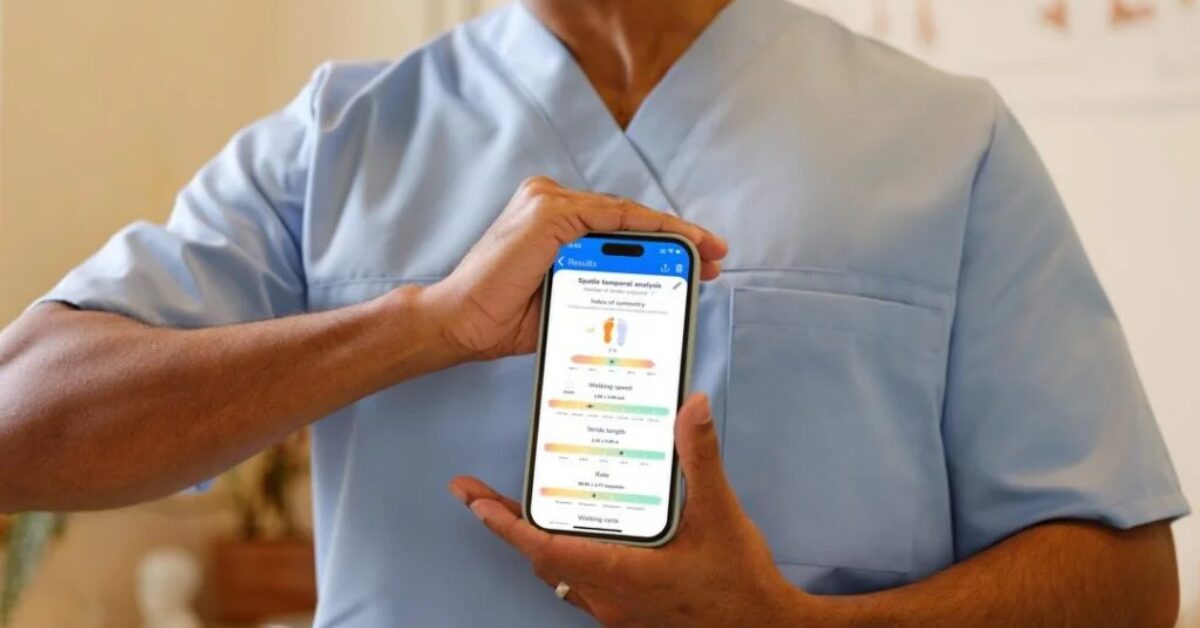
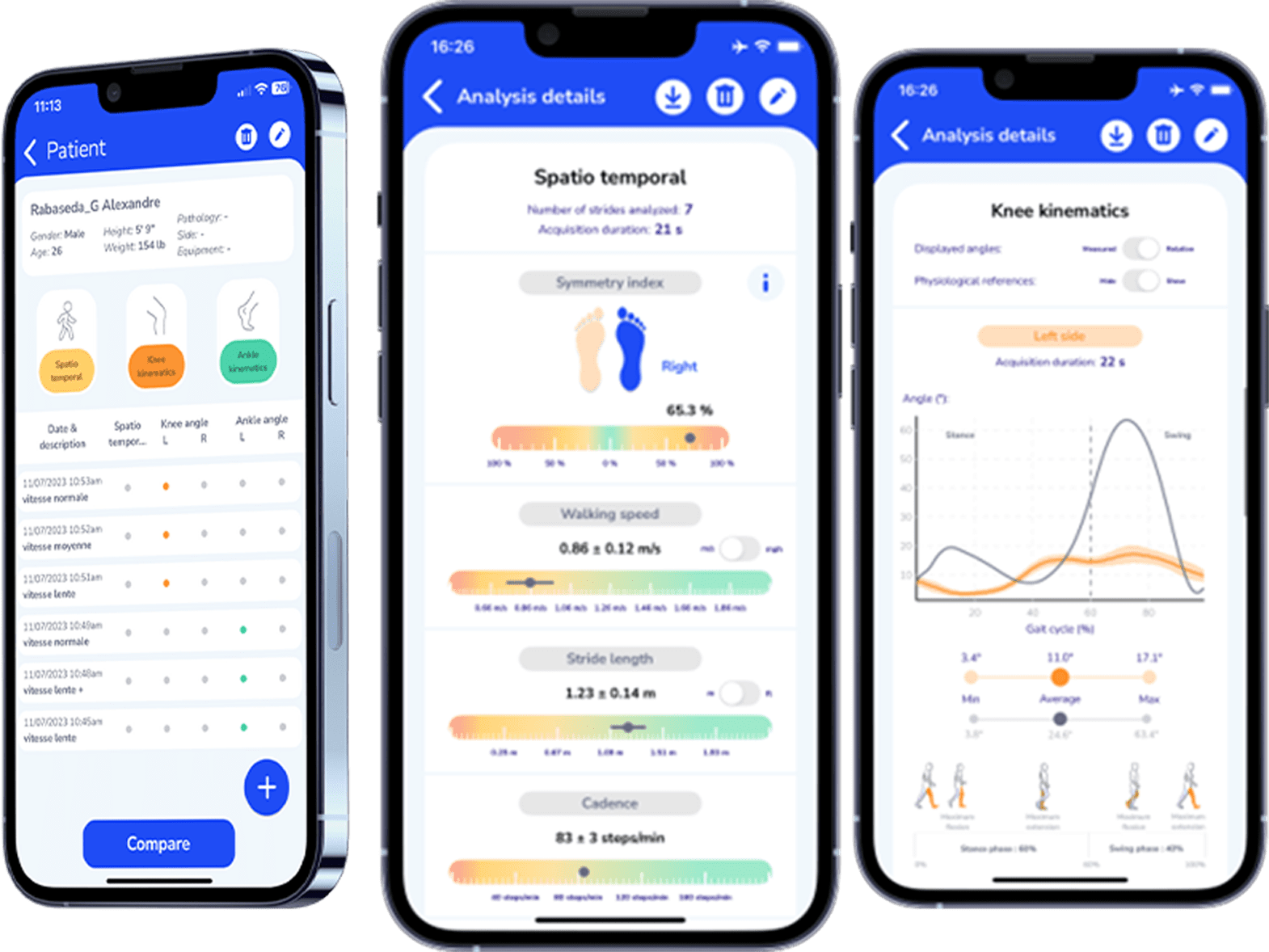
Fall prevention is complex. No single assessment or intervention can guarantee a patient won’t fall. However, REEV’s gait analysis software, SENSE, provides objective gait data that identifies gait patterns associated with an increased fall risk. Then, PTs can address these risks through treatment, referrals, or equipment such as the DREEVEN robotic knee orthosis.

Using Objective Gait Data to Identify Patients at Risk for Falls
The first way gait analysis technology supports care is by helping PTs identify which patients are at risk for falls.
Clinicians use a variety of methods to identify fall risk, including balance tests like the Berg Balance Scale, walking speed, self-report questionnaires, skilled observation, and the Timed Up and Go (TUG).
While these approaches are valuable, they also have limitations. Results vary between clinicians, subtle changes may go unnoticed, and patients may perform differently when they know they are being assessed. In addition, self-report is not always reliable, as patients may lack insight into their own limitations or minimize concerns.
Objective gait data collected through sensor technology offers a more concrete way to assess fall risk. Well-designed gait technology provides clear numerical values of deficits and even small amounts of progress.
When determining fall risk, PTs can use quantifiable gait metrics like gait speed, asymmetry, and step length. This type of data is especially important when working with a patient post-stroke with lower extremity weakness on the affected side.

Patient Education and Buy-In Around Fall Risk
Insights into their fall risk and ability to improve directly impact whether a patient will seek out fall-prevention interventions, implement recommended activities, or use equipment such as a walker or the DREEVEN robotic knee brace.
There are two directions patients lean when it comes to fall risk:
- Some patients are so fearful of falling that they drastically restrict their activity in an attempt to reduce their fall risk. This reduced activity actually leads to weakness and an even greater risk for falls.
- Other patients deny or underestimate their risk and resist recommendations for therapy or safety changes. They reject equipment and engage in unsafe activities, which increases their fall risk.
Data allows clinicians to provide patients with a clear, accurate picture of their performance and risk level. PTs can compare a patient’s scores to fall risk data and show changes over time, making the risk more concrete and tangible.
This data-driven approach using real-time feedback increases buy-in. Patients are more likely to follow through with therapy, perform home exercises, use assistive devices, or make environmental modifications when they understand why it matters and that their actions make a difference.
Implement a Targeted, Fall Prevention Exercise Program
Exercise is one of the most effective interventions for reducing fall risk because it addresses modifiable contributors such as strength, balance, coordination, and walking speed. PTs develop exercise programs to target specific functional deficits, such as stance symmetry or stride length. These gait metrics can be measured with the SENSE gait analysis software.
Some older adults believe that they can’t meaningfully improve their strength or balance, especially if they’ve had a stroke. Many patients won’t complete their home exercise program independently. Gait assessment technology can provide proof of progress, which then increases their motivation and participation in their exercise program.
PTs can also follow up with patients in the clinic and through Remote Therapeutic Monitoring to encourage participation and help patients see how the improvements are affecting their daily activities.

Data-Driven Fall Prevention as a PT Practice Asset
While improved clinical outcomes are the primary driver of fall prevention programs, objective gait data also plays an important role in strengthening the business foundations of physical therapy practice.
Incorporating objective gait analysis into fall prevention supports:
- Enhanced patient retention: Patients who see measurable progress are more likely to stay engaged in care or return in the future.
- Increased referrals: Families and caregivers recognize the value of proactive fall prevention intervention, making them more likely to refer friends and family.
- Reimbursement support: Objective data demonstrates deficits and improvements, which can reduce denials, appeals, and administrative burden.
- Reduced liability: Comprehensive identification of fall risk supports safer care delivery and helps prevent patient falls and injuries within the clinic or facility.
Objective gait analysis bridges clinical effectiveness and business sustainability by aligning measurable outcomes with organizational goals in fall prevention.
Enhancing Fall Prevention Through Gait Analysis Technology
No patient wants to fall, and no PT wants to see a patient return to therapy due to a fall. Proactively working to prevent falls is how injuries, hospitalizations, and loss of independence can be minimized. Objective gait metrics add meaningful value to fall risk assessment and prevention programs. The data enhances clinical insight, improves patient education and buy-in, supports targeted interventions, and provides clear evidence of progress and outcomes.
REEV supports a data-driven and comprehensive approach to fall prevention through a complete mobility platform that includes easy-to-use, accurate gait analysis technology and DREEVEN, an advanced, motorized knee brace.
References:
Stevens, J. A., Sleet, D. A., & Rubenstein, L. Z. (2017). The Influence of Older Adults’ Beliefs and Attitudes on Adopting Fall Prevention Behaviors. American journal of lifestyle medicine, 12(4), 324–330. https://pmc.ncbi.nlm.nih.gov/articles/PMC6993092/
Quach, L., Galica, A. M., Jones, R. N., Procter-Gray, E., Manor, B., Hannan, M. T., & Lipsitz, L. A. (2011). The Non-linear Relationship between Gait Speed and Falls: The MOBILIZE Boston Study. Journal of the American Geriatrics Society, 59(6), 1069. https://pmc.ncbi.nlm.nih.gov/articles/PMC3141220/
Kim, U., Lim, J., Park, Y. et al. Predicting fall risk through step width variability at increased gait speed in community dwelling older adults. Sci Rep 15, 16915 (2025). https://doi.org/10.1038/s41598-025-02128-2
Jordyn Rice, Ryan S Falck, Jennifer C Davis, Chun L Hsu, Larry Dian, Kenneth Madden, Naaz Parmar, Wendy L Cook, Karim M Khan, Teresa Liu-Ambrose, Gait Speed Modifies Efficacy of Home-Based Exercise for Falls in Older Adults With a Previous Fall: Secondary Analysis of a Randomized Controlled Trial, Physical Therapy, Volume 105, Issue 3, March 2025, pzaf008, https://academic.oup.com/ptj/article/105/3/pzaf008/7989354
Florence CS, Bergen G, Atherly A, Burns ER, Stevens JA, Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. Journal of the American Geriatrics Society, 2018 March, DOI: 10.1111/jgs. 15034